Living with Chronic Obstructive Pulmonary Disease (COPD) involves managing your day-to-day symptoms. However, sometimes those symptoms can suddenly worsen, leading to a serious health event known as a flare-up or exacerbation. These episodes can be frightening and may even require hospitalization.
Understanding what a flare-up is, recognizing its early warning signs, and knowing how to respond when one occurs can make a significant difference in your health and overall quality of life.
This guide will walk you through the essential steps for managing COPD exacerbations, from creating a personalized action plan to prevent future flare-ups. Learning to take control can help you breathe more easily and reduce the need for hospitalization.
What is a COPD Flare-Up?
A COPD flare-up, or exacerbation, is a period when your respiratory symptoms become more severe than usual. It’s not just a “bad day”—it’s a distinct worsening of your condition that can last for several days or even weeks. During a flare-up, inflammation in your airways increases, leading to more mucus production and making it much harder to breathe.
The most common cause of a flare-up is a respiratory infection, like a cold or the flu. Other triggers can include exposure to air pollution, smoke, or other lung irritants. These events are not only uncomfortable but can also cause permanent lung damage, accelerating the progression of COPD. This is why recognizing and treating flare-ups early is so important.
Recognizing Early Warning Signs
The first step in managing a flare-up is to recognize the signs and symptoms to look for. Symptoms can vary from person to person, but there are common warning signs that indicate an exacerbation may be starting. Paying close attention to your body and how you feel each day will help you catch these changes early.
Common early warning signs include:
- Increased Shortness of Breath: You find it harder to breathe than usual during your daily activities.
- More Coughing: You’re coughing more frequently, or your cough sounds different.
- Changes in Mucus: You notice an increase in the amount of mucus, or it changes color (e.g., to yellow, green, or brown) or thickness.
- Wheezing: You experience more wheezing or a whistling sound when you breathe.
- Fatigue: You feel unusually tired or have less energy.
- Swelling: You notice new or worsening swelling in your ankles, feet, or legs.
- Confusion or Drowsiness: These can be signs of low oxygen levels and require immediate attention.
Self-monitoring is key. By tracking your symptoms daily, you can establish a baseline for what is “normal” for you, making it easier to spot when something is wrong.
Why Early Action is Crucial
When you notice the early signs of a flare-up, acting quickly is vital. Prompt treatment can help you manage the exacerbation at home and may prevent the need for a trip to the emergency room. Delaying action can allow the symptoms to spiral out of control, leading to severe breathing difficulties, low oxygen levels, and the need for hospitalization.
Early intervention often involves adjusting your medications according to a pre-arranged plan, contacting your doctor, and getting plenty of rest. By taking these steps, you can reduce the severity and duration of the flare-up and minimize its impact on your long-term lung health.
Your COPD Action Plan
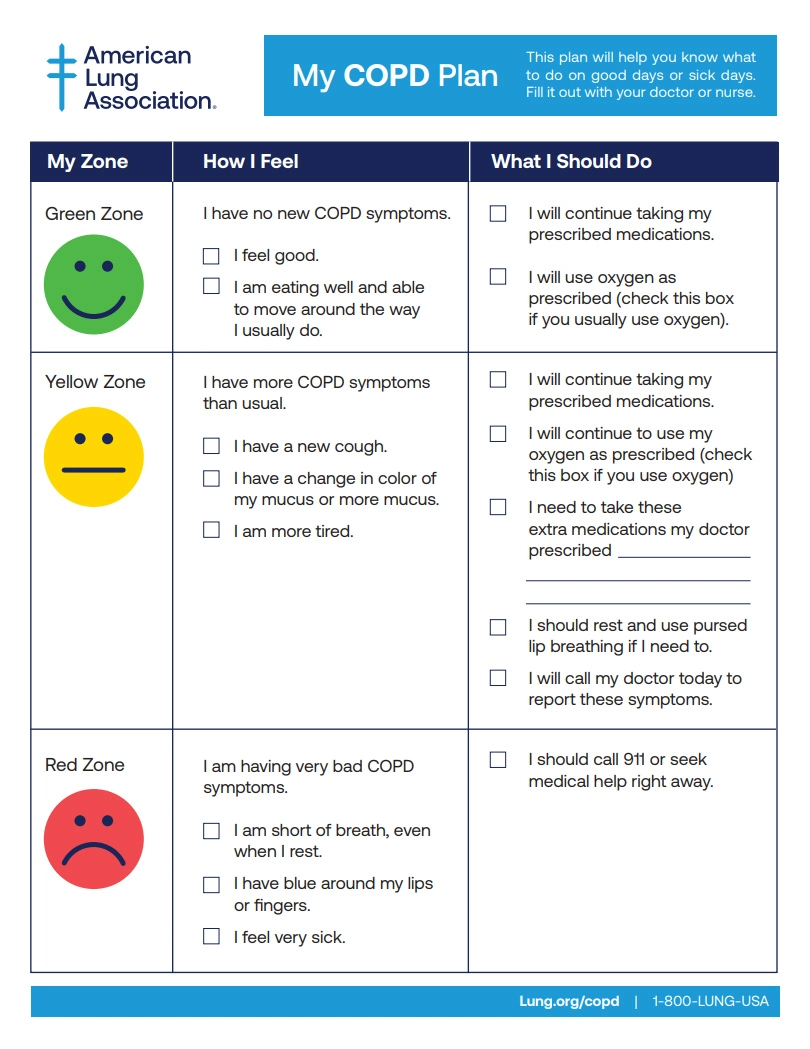
One of the most effective tools for managing flare-ups is a COPD Action Plan. This is a written document that you create with your healthcare provider. It tells you exactly what to do based on your symptoms, using a simple traffic light system: Green, Yellow, and Red.
What is an Action Plan?
A COPD Action Plan empowers you to take control of your health. It provides clear, personalized instructions for daily management and for handling worsening symptoms. Let’s break down what each zone means.
Green Zone: “I Am Doing Well”
The Green Zone describes your day-to-day state when your COPD is well-managed. In this phase, you should:
- Continue taking your regular maintenance medications as prescribed.
- Engage in your usual daily activities and exercise routine.
- Your breathing is at its normal level, and you feel good.
This is your baseline. The goal is to stay in the Green Zone as much as possible.
Yellow Zone: “Caution – Flare-Up Starting”
The Yellow Zone indicates that you are experiencing a flare-up. You’ve noticed one or more of the early warning signs, like increased shortness of breath or changes in your mucus. Your action plan will tell you exactly what to do, which may include:
- Using your quick-relief (rescue) inhaler as directed by your provider.
- Starting an oral steroid (like prednisone) or an antibiotic that your doctor has prescribed for you to keep on hand.
- Practicing breathing techniques, like pursed-lip breathing, to ease shortness of breath.
- Calling your doctor’s office to let them know about your symptoms.
The specific instructions in your Yellow Zone plan will be tailored to your medical history and needs.
Red Zone: “Medical Alert – Emergency”
The Red Zone signifies a severe flare-up that requires immediate medical attention. Symptoms in this zone are serious and can be life-threatening. Your action plan will instruct you to:
- Call 911 or go to the nearest emergency room.
- Symptoms indicating a Red Zone emergency include:
- Severe shortness of breath, even at rest.
- Difficulty speaking in full sentences.
- Confusion, drowsiness, or disorientation.
- Chest pain.
- Blue or gray lips or fingertips.
Do not wait to seek help if you are in the Red Zone. Emergency medical care is necessary to stabilize your breathing and prevent serious complications.
Working With Your Healthcare Team
Your relationship with your healthcare team is a partnership. To effectively manage your COPD, you need to work closely with your doctor, pulmonologist, and respiratory therapist.
Be open and honest about your symptoms, your lifestyle, and any challenges you face in managing your condition. When creating your action plan, ask questions to ensure you understand every step. Regular check-ups are also essential, even when you are feeling well. These appointments are an opportunity to review your action plan, adjust medications, and discuss any concerns.
Preventing Future Flare-Ups
While not all flare-ups can be avoided, there are many proactive steps you can take to reduce your risk. Prevention is the best medicine and is a crucial part of your long-term COPD management.
Key prevention strategies include:
- Get Vaccinated: Stay up-to-date on your flu shot, pneumonia vaccine, RSV, and COVID-19 boosters.
- Wash Your Hands: Frequent handwashing is one of the best ways to avoid respiratory infections.
- Avoid Lung Irritants: Stay away from tobacco smoke, dust, strong fumes, and air pollution as much as possible.
- Take Medications as Prescribed: Adhering to your daily maintenance medication schedule is vital for keeping your airways open and inflammation down.
- Stay Active: Regular exercise, as approved by your doctor, can strengthen your breathing muscles and improve your overall health.
- Eat a Healthy Diet: Good nutrition supports your immune system and provides the energy you need to stay active.
Take Charge of Your Breathing
Living with COPD presents daily challenges but understanding how to manage flare-ups can empower you to lead a fuller, more active life. By recognizing early symptoms, following a personalized action plan, and working with your healthcare team, you can gain greater control over your condition.
Taking proactive steps to prevent exacerbations is just as important, helping you protect your lung function for the long term.
If you don’t have a COPD Action Plan, schedule an appointment with your doctor to create one. It’s one of the most important things you can do for your health.